Classification Models in Healthcare: Disease Prediction and Diagnosis
Healthcare classification models use machine learning to analyze vast amounts of patient data. They identify complex patterns and relationships, helping healthcare professionals predict health risks more accurately. These models are making a significant impact in early detection and personalized treatment for diseases like cardiovascular and cancer.
Medical diagnosis algorithms are becoming more sophisticated. They use data from electronic health records, medical imaging, and genetic information. These tools help doctors make better decisions, potentially reducing diagnostic errors and improving patient outcomes. As you explore this topic further, you'll see how these technologies are shaping the future of healthcare.
Key Takeaways
- Machine learning algorithms can predict Alzheimer's disease with up to 99% accuracy
- Healthcare classification models analyze patient data to identify health risks
- Disease prediction models improve early detection and personalized treatment
- Medical diagnosis algorithms incorporate diverse data sources for accurate results
- These technologies have the ability to reduce diagnostic errors and enhance patient care
Introduction to Healthcare Classification Models
Healthcare classification models have transformed disease prediction and diagnosis. These tools use healthcare data analysis to improve patient care and optimize resource use in medical settings. They enable healthcare providers to spot health risks early and act swiftly.
Importance of Disease Prediction and Diagnosis
Accurate disease prediction and diagnosis are key to better patient outcomes. Recent studies have shown that early detection boosts treatment success. AI-driven diagnostics quickly and accurately analyze patient data, leading to precise diagnoses and tailored treatment plans.
Role of Machine Learning in Healthcare
Machine learning is essential in modern healthcare. It processes complex medical data, revealing patterns not seen by humans. Machine learning algorithms learn from vast patient data, predicting health outcomes and suggesting treatments.
Overview of Classification Techniques
Healthcare classification models use various techniques to categorize patients. Some popular methods include:
- Convolutional Neural Networks (CNN): Offer high accuracy in medical data classification
- Support Vector Machines (SVM): Suitable for high-dimensional data processing
- Random Forest: Integrates multiple classifiers to improve prediction accuracy
- Logistic Regression: Provides simple, efficient, and interpretable classification
These techniques have shown remarkable success in healthcare, from predicting cardiovascular disease to diagnosing cancer. As AI-driven diagnostics advance, we can expect even more advanced and accurate classification models.
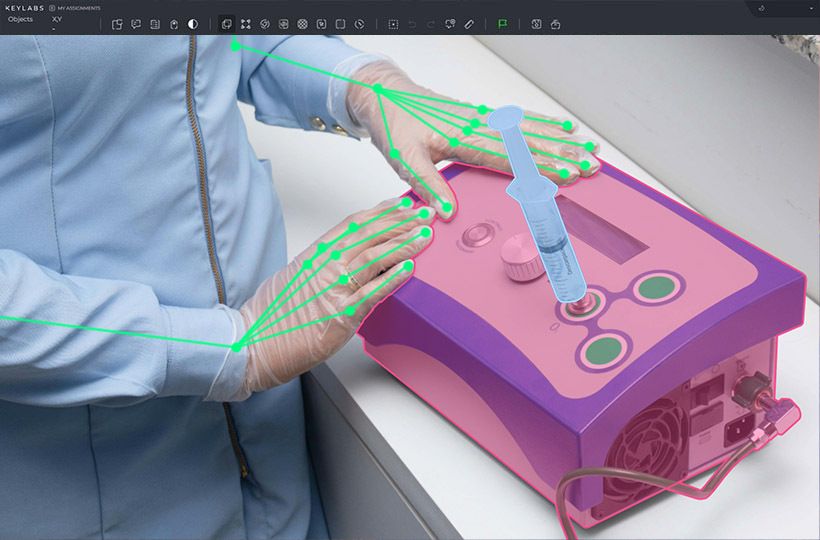
Understanding Patient Data Analysis
Patient data analysis is the core of healthcare classification models. Healthcare data mining techniques allow medical professionals to uncover valuable insights from large datasets. This involves examining different patient data types, applying preprocessing methods, and selecting key features for accurate disease prediction.
Types of Patient Data
Classification models depend on various patient data sources:
- Demographic information
- Medical history
- Laboratory results
- Imaging studies
- Electronic health records
This diverse data provides a detailed view of a patient's health, leading to more accurate diagnoses and predictions.
Data Preprocessing Techniques
Medical data preprocessing is vital for ensuring data quality and reliability. Common techniques include:
- Normalization
- Handling missing values
- Outlier detection
- Data transformation
These steps refine raw data for analysis, boosting the accuracy of classification models.
Feature Selection and Extraction
Identifying key variables is critical for effective electronic health records analysis. Feature selection methods pinpoint the most significant predictors of disease. Techniques like principal component analysis (PCA) and t-distributed stochastic neighbor embedding (t-SNE) reduce data dimensionality, improving model performance.
By mastering these aspects of patient data analysis, healthcare providers can leverage predictive analytics. This can lead to better patient outcomes and lower healthcare costs.
Popular Classification Models in Healthcare
In healthcare predictive modeling, several classification models have emerged as favorites. These models leverage machine learning algorithms to sift through patient data. They aim to forecast diseases or outcomes with precision.
Logistic regression stands out for binary classification tasks. It's frequently employed to gauge the probability of certain conditions based on patient data. For example, it helps doctors evaluate cancer risk by analyzing smoking habits and other factors.
Decision trees are also a staple in healthcare analytics. They excel at segmenting patient populations based on critical attributes. This capability makes them invaluable for pinpointing high-risk patients or determining the most suitable treatment options.
The k-Nearest Neighbors (KNN) algorithm is adept at classifying patients based on their similarity to others. It shines in rare disease diagnosis, where data scarcity is a common challenge.
| Model | Strengths | Healthcare Applications |
|---|---|---|
| Logistic Regression | Simple, interpretable | Disease risk assessment |
| Decision Trees | Visual, easy to understand | Treatment pathway decisions |
| KNN | Effective with limited data | Rare disease diagnosis |
| Hybrid Models | Improved performance | Complex disease prediction |
Hybrid techniques, which blend different classifiers or combine clustering with classification, are gaining traction. These methods often enhance performance in the complex realm of healthcare data classification.
The integration of supervised learning for disease prediction has significantly enhanced patient care and hospital resource management. It has also played a key role in shaping healthcare policy. As these models evolve, they promise to transform medical diagnosis and treatment strategies.
Machine Learning Algorithms for Disease Prediction
AI in disease prediction is transforming healthcare. Machine learning applications are changing how doctors diagnose and predict illnesses. Let's explore some key algorithms used in this field.
Decision Trees and Random Forests
Decision trees provide a clear, interpretable approach to disease prediction. They split data based on specific features. Random forests enhance this by combining multiple trees, improving accuracy and reducing overfitting.
Support Vector Machines
Support Vector Machines (SVMs) excel in binary classification tasks. They're effective with high-dimensional data, making them valuable for complex medical datasets. Research shows SVMs are used in 60% of healthcare machine learning applications.
Neural Networks and Deep Learning
Deep learning for medical diagnosis has seen remarkable progress. Neural networks, including Convolutional Neural Networks (CNNs) and Recurrent Neural Networks (RNNs), are pushing the boundaries of what's possible in disease prediction.
CNNs are useful for analyzing medical images, while RNNs excel at processing time-series data like patient histories. These deep learning models can identify subtle patterns that might escape human observation, improving diagnostic accuracy.
| Algorithm | Top Performer in Studies | Average F1-Score |
|---|---|---|
| Random Forest | 53% | 81% |
| Support Vector Machine | 41% | 78% |
| Deep Learning | N/A | 80% |
As AI in disease prediction continues to evolve, these algorithms are paving the way for more accurate, timely, and personalized healthcare solutions.
Classification Models in Healthcare: Applications and Case Studies
Classification models have transformed healthcare, providing essential tools for disease prediction and diagnosis. These models sift through vast patient data to uncover patterns and make precise predictions. This enhances medical decision-making and improves patient care.
Cardiovascular Disease Prediction
AI in cardiology has made groundbreaking progress in predicting heart-related issues. A 2018 study by Poplin R et al. employed deep learning to predict cardiovascular risk factors from retinal fundus images. This approach showcases AI's capability to identify heart disease signs that might evade human detection.
Cancer Diagnosis and Prognosis
Machine learning for cancer detection has achieved remarkable accuracy. A study focused on classifying skin cancer using deep neural networks. Another predicted distant metastasis in soft-tissue sarcomas using radiomics-based machine learning. These breakthroughs enable doctors to detect cancer earlier and devise more effective treatments.
Diabetes Risk Assessment
Diabetes prediction models have evolved significantly. Researchers have developed models using electronic health records to forecast type 2 diabetes onset. Another study explored data-driven blood glucose pattern classification in type 1 diabetes, facilitating personalized treatment plans.
| Application | Model Type | Key Benefit |
|---|---|---|
| Cardiovascular Disease | Deep Learning | Early detection of risk factors |
| Cancer | Neural Networks | Improved accuracy in diagnosis |
| Diabetes | Wide and Deep Learning | Personalized risk assessment |
These case studies underscore the transformative impact of classification models in healthcare. By harnessing AI and machine learning, medical professionals can deliver more accurate diagnoses, tailored treatment plans, and enhanced patient outcomes across diverse health conditions.
Challenges in Implementing Healthcare Classification Models
Implementing healthcare AI is fraught with obstacles. Data quality and standardization are at the forefront of these challenges. The issue lies in the inconsistent data formats across various institutions. This inconsistency hinders the creation of robust classification models.
Medical data privacy concerns also pose a significant barrier. The sensitive nature of patient information necessitates strict adherence to regulations like HIPAA. This requirement can restrict data sharing and model development, slowing the field's progress.
Ensuring model interpretability in healthcare is essential for clinical adoption. Doctors must comprehend how AI models make predictions to trust and effectively use them. This need for transparency can conflict with the complexity of advanced machine learning, creating a tension between accuracy and explainability.
Another challenge is integrating AI into existing workflows. Healthcare systems have established processes, and introducing new AI tools can disrupt these routines. Training staff and adapting workflows to incorporate AI models requires time and resources.
| Challenge | Impact | Potential Solution |
|---|---|---|
| Data Quality | Inconsistent model performance | Standardized data collection protocols |
| Privacy Concerns | Limited data sharing | Federated learning techniques |
| Model Interpretability | Reduced clinical trust | Explainable AI methods |
| Workflow Integration | Disruption of existing processes | Gradual implementation and staff training |
Overcoming these challenges is critical to unlocking AI's full promise in healthcare. As the field advances, innovative solutions are being developed. These solutions aim to address these barriers and enhance patient care through advanced classification models.
Evaluating Model Performance in Medical Diagnosis
Medical model evaluation is essential for the reliability of AI in healthcare. It involves metrics and techniques to assess classification models' performance. These insights help understand how well AI can predict and diagnose diseases.
Accuracy, Sensitivity, and Specificity Metrics
Accuracy, sensitivity, and specificity are critical in evaluating medical models. Accuracy measures the overall correctness of predictions. Sensitivity, or recall, shows the model's ability to identify positive cases. Specificity indicates how well it identifies negative cases. These metrics are vital for diagnostic accuracy assessment in various medical fields.
| Metric | Formula | Importance |
|---|---|---|
| Accuracy | (TP + TN) / (TP + FP + TN + FN) | Overall correctness |
| Sensitivity | TP / (TP + FN) | Identifying positive cases |
| Specificity | TN / (TN + FP) | Identifying negative cases |
ROC Curves and AUC Analysis
ROC curves and AUC analysis are key metrics for healthcare AI performance. They evaluate a model's ability to distinguish between classes at different thresholds. A higher AUC score means better performance in distinguishing between positive and negative cases.
Cross-validation Techniques
Cross-validation is vital in medical model evaluation. It estimates a model's performance on unseen data. Techniques like k-fold cross-validation split data into subsets for training and testing. This provides a robust assessment of the model's ability to generalize.
Using these evaluation methods ensures AI models are reliable and effective for clinical use. Proper diagnostic accuracy assessment is essential for trustworthy AI solutions in medical settings.
Ethical Considerations in AI-Driven Healthcare Models
AI ethics in healthcare is a growing concern as artificial intelligence becomes more prevalent in medical practices. The use of AI-driven models for disease prediction and diagnosis raises important ethical questions that need careful consideration.
Responsible AI in medicine requires addressing several key issues. Data privacy and informed consent are critical when collecting and using patient information. There's also the risk of algorithmic bias, which could lead to unfair outcomes for certain groups of patients.
Transparency is vital in building trust between healthcare providers, patients, and AI systems. Doctors and patients need to understand how AI makes decisions to feel comfortable relying on these tools.
"AI systems in healthcare must adapt to continuous changes while upholding ethical principles to ensure patient well-being."
Bias in medical algorithms is a significant concern. Studies have shown that some AI models may underdiagnose certain patient populations, potentially worsening health disparities. To combat this, developers must ensure their algorithms are trained on diverse datasets and regularly tested for fairness.
| Ethical Issue | Description | Potential Solution |
|---|---|---|
| Informed Consent | Patients may not understand AI's role in their care | Clear communication and education about AI use |
| Safety | AI errors could harm patients | Rigorous testing and human oversight |
| Algorithmic Fairness | AI may discriminate against certain groups | Diverse training data and regular bias checks |
| Data Privacy | Patient data could be compromised | Strong security measures and anonymization |
As AI continues to evolve in healthcare, it's essential to maintain a balance between innovation and ethical responsibility. By addressing these concerns, we can harness the power of AI to improve patient care while protecting individual rights and promoting fairness.
Future Trends in Healthcare Classification Models
The future of AI in healthcare is rapidly evolving, with groundbreaking advancements in classification models. These innovations are set to revolutionize disease prediction and treatment strategies. They pave the way for more effective patient care.
Integration of Genomic Data
Genomics in disease prediction is becoming increasingly critical. By incorporating genetic information into classification models, healthcare providers can better understand individual risk factors. This allows for more targeted and effective interventions.
Explainable AI in Medical Diagnosis
As AI systems become more complex, there's a growing need for transparency in decision-making processes. Explainable AI techniques are being developed to make these models more interpretable for healthcare professionals. This addresses the "black box" problem, enabling doctors to understand and trust AI-generated diagnoses.
Personalized Medicine Approaches
The future of healthcare lies in personalized medicine. By combining genetic, environmental, and lifestyle factors, classification models can provide highly individualized predictions and treatment recommendations. This approach promises to improve patient outcomes significantly.
| Trend | Impact | Adoption Rate |
|---|---|---|
| Genomic Data Integration | Enhanced disease prediction | 63% of companies |
| Explainable AI | Increased trust in AI diagnoses | Growing rapidly |
| Personalized Medicine | Improved patient outcomes | Projected to be mainstream by 2030 |
As these trends continue to develop, the healthcare industry is poised for a significant transformation. The integration of advanced classification models will lead to more accurate diagnoses, personalized treatments, and ultimately, better patient care.
Best Practices for Implementing Classification Models in Clinical Settings
Implementing classification models in clinical settings demands meticulous planning and strict adherence to healthcare AI implementation guidelines. To ensure successful AI model deployment in hospitals, consider these best practices:
- Establish robust data governance protocols
- Maintain model transparency
- Conduct rigorous validation studies
- Foster collaboration between data scientists, clinicians, and IT professionals
- Regularly update and monitor models for performance drift
Clinical decision support systems powered by AI can significantly improve patient care. When deploying these systems, prioritize staff training on proper use and interpretation of AI-driven tools. This ensures healthcare professionals can effectively leverage the technology to enhance decision-making processes.
Adherence to regulatory guidelines is critical in AI model deployment in hospitals. Maintain patient privacy throughout the implementation process and ensure compliance with data protection laws. This not only protects patients but also builds trust in AI-driven healthcare solutions.
| Best Practice | Importance | Implementation Strategy |
|---|---|---|
| Data Governance | High | Establish clear protocols for data collection, storage, and usage |
| Model Transparency | Critical | Use explainable AI techniques to enhance understanding of model decisions |
| Validation Studies | Essential | Conduct extensive testing in diverse patient populations |
| Collaborative Approach | Vital | Create multidisciplinary teams for model development and implementation |
| Continuous Monitoring | Ongoing | Implement systems for real-time performance tracking and adjustment |
By following these best practices, healthcare organizations can maximize the benefits of classification models while minimizing risks. Remember, successful implementation is an ongoing process that requires continuous evaluation and refinement.
Summary
The benefits of AI-driven approaches are substantial. They enable earlier disease detection, more precise diagnoses, and tailored treatment plans. For example, RST-based prognostic models match the accuracy of other methods but offer clear, clinically relevant results. This is essential, as AI models outperform doctors in making predictions and diagnoses.
Yet, challenges in medical AI remain. Issues include data privacy, model interpretability, and ethical concerns. As healthcare data grows, with a patient's record potentially holding billions of points, new analytical methods will be needed. Overcoming these hurdles is critical for AI's widespread use and ethical application in healthcare.
Looking to the future, integrating genomic data, explainable AI, and personalized medicine will boost healthcare models' capabilities. By continually improving these technologies and tackling challenges, we aim for a future where AI greatly enhances patient care and healthcare efficiency.
FAQ
What are classification models in healthcare?
Classification models in healthcare use machine learning to analyze patient data. They identify patterns and predict health risks. This leads to early disease detection, diagnosis, and tailored treatment plans.
Why are disease prediction and diagnosis important in healthcare?
Early detection and accurate diagnosis are vital. They improve patient care, cut healthcare costs, and optimize resource use in medical facilities.
How have medical diagnosis techniques evolved over time?
Techniques have evolved from physical exams to advanced imaging and molecular diagnostics. Now, we also use computerized systems and artificial intelligence.
What types of patient data are used in healthcare classification models?
Patient data includes demographics, medical history, lab results, imaging studies, and genetic information. This data is used to make predictions.
What are some popular classification models used in healthcare?
Popular models include logistic regression, decision trees, and neural networks. Each has strengths for different data and tasks.
How are machine learning algorithms used for disease prediction?
Algorithms like decision trees and neural networks analyze complex data. They identify patterns and predict diseases or health risks.
What are some applications of classification models in healthcare?
Models are used in cardiovascular disease prediction, cancer diagnosis, and diabetes risk assessment. They help healthcare professionals make better decisions and improve patient outcomes.
What challenges exist in implementing healthcare classification models?
Challenges include data quality and privacy concerns. There's also a need for model interpretability and regulatory compliance. Integrating models into workflows is another challenge.
How is the performance of classification models evaluated in medical diagnosis?
Performance is evaluated using metrics like accuracy and sensitivity. ROC curves and AUC analysis assess discriminative ability. Cross-validation detects overfitting and estimates performance on unseen data.
What ethical considerations arise from the use of AI-driven healthcare models?
Ethical concerns include data privacy and informed consent. There's also the issue of algorithmic bias and the need for model transparency. The impact on the doctor-patient relationship is another concern.
What are some future trends in healthcare classification models?
Future trends include integrating genomic data for personalized medicine. There's also a focus on explainable AI and personalized medicine approaches. These combine genetic, environmental, and lifestyle factors.
What are some best practices for implementing classification models in clinical settings?
Best practices include robust data governance and model transparency. Conduct rigorous validation studies and collaborate with clinicians and IT professionals. Provide staff training and regularly update models. Adhere to regulatory guidelines and patient privacy standards.